Get a FREE
ENU Intro Pack*
*Just Pay $2.00 Shipping
Optimizing Nutrition During Cancer Treatment: Preventing & Managing Malnutrition
This post is an excerpt of a recent webinar titled, “Optimizing Nutrition During Treatment: Preventing & Managing Malnutrition” by Julie Lanford, MPH, RD, CSO, LDN, in which she discusses strategies for meeting nutrition needs during treatment. To view the full video, please click on the thumbnail below:
In this blog post, we are going to cover these five things: 1) The role of nutrition during treatment, 2) malnutrition during cancer treatment, 3) general tips for general nutrition and nutrition during treatment, 4) common treatment side effects, and 5) ENU Nutrition products that can help people during treatment.
So this is, if any of you have attended my other webinars, I use some of the same slides over and over again, and this is one of them. So, I find that, when I’m working with patients, I need to sort of assess where they are or make sure that we’re on the same page in terms of what they’re expecting nutrition is going to do for them during treatment versus what I think that I’m going to be helping them with. I like to make sure that we’re all on the same level of understanding in terms of what is the role of nutrition during treatment. So, this is my fancy picture (you can see I’m quite the artist), and the yellow circle is our whole person, and then the cancer is represented by the grey circle inside.
So remembering that a person may have cancer – but that doesn’t, you know, make up their whole self – and to remind people that nutrition is not a cure for cancer but that nutrition does play a role in supporting and maintaining all the cells of the body. So, really helping them realize that when we tailor their nutrition strategy, it’s more about helping to make sure their whole body can essentially tolerate the treatments and to come out on the other side of treatment as healthy and healed up as well as possible, whereas the treatments themselves in terms of chemo, radiation, surgery, hormone therapy – they’re very targeted to the tumor.
I find some of my patients, they come to me thinking, “Well, I really want to cure my cancer with diet, and that’s something that we have to kind of work through is to maybe alter expectations or talk about whether what they’re thinking nutrition is going to do for them is really what we’re going for.
I often start with (even if we’re not quite on the same page) I talk about what does nutrition do for them, so what is it that they can expect. We would expect that, if we can maintain good nutrition status, side effects will be lessened; we can expect that their immune system will be supported as much as possible. Ideally, we’re hoping to maintain weight, or at least kind of keep weight loss at a minimum, and also to optimize the amount of energy they have. So, of course there’s no guarantees that by having good nutrition they’ll all of a sudden have all this energy, because they’re going through cancer treatment. That’s a lot to expect, but certainly, if you’re not well-nourished and you’re going through cancer treatment, you’re not going to feel as well as if you could maintain nutrition as much as possible.
So, what it can’t do is cure cancer. And I have had phone calls as, you know, the dieticians on here also probably have as well, that a patient who’s trying to decide, they don’t really want to do chemo, the don’t really want to deal with the side effects of treatment, and they’d rather just cure it with diet. And those I try to be pretty clear that that, first of all, is not what I do as a dietician, but that data doesn’t suggest that’s possible. So what we want to make sure is that people’s expectations are on the same page and that we’re working toward the same goals.
Nutrition Needs During Cancer Treatment
Alright, so, nutrition during treatment. The other thing that I can help patients often understand is that, if they are malnourished, that’s going to decrease their immune response; it’s going to contribute to fatigue – which, many cancer patients face fatigue – decrease their muscle strength, it affects their ability to tolerate treatment – that affects their quality of life – their ability to function within their social circles (which are a little bit tight right now), and also affect their wound healing, especially that wound healing piece. If people are going through surgeries, it’s really important that they key in on their nutrition needs.
So, this is another way I often describe it to people is understanding that there’s a cycle that sort of goes on around malnutrition or adequate nutrition, and we want to meet nutrition needs, provide adequate nutrition for a variety of reasons, and this is the cycle that makes sense to me. By meeting our nutrition needs or getting enough calories and protein, that helps to build or maintain energy stores so your body is able to add to stores and meet nutritional needs. Usually, that means that your weight is stable, and that means that your immune system is supported, you have more energy, treatments are tolerable, blood counts are stable, and therefore we have our best chance at good outcomes.
So, this is kind of the ideal picture, right? Of course we know, “OK, yeah, of course, you get the dietician or you get the patient who can eat well, and things just go well.” The problem is that this is what often happens in cancer, and this is why we have oncology dieticians, and ideally, cancer centers would have one available – outpatient – to help people with this, to intervene early. So, this is the cycle that happens if somebody is not able to get enough food. Their calorie and protein needs are not met, which means their body has to pull off energy stores, and they might be using up fat stores, using up muscle stores, to meet their nutrition needs; that results in weight loss.
Often times, that’s fat or muscle loss, which is – especially during treatment – not what we want, and I know somebody sent a question ahead of time, which is about sometimes patients are actually maybe secretly happy about losing weight, and so we’ll talk about that in a little bit. But usually, it’s not a good sign during cancer treatment, because that leaves you feeling weak and tired; it means your immune system is not supported; you’re fatigued. You might miss treatments because your body’s not strong enough to tolerate them, your counts are low, and then treatment is less effective.
Preventing Malnutrition During Cancer Treatment
I find a lot of time, you know, patients really haven’t, I don’t know, people haven’t taken the time to educate them as to why nutrition plays a key role in making sure that they don’t miss treatments. And sometimes, their team, they’re working really hard to make sure they don’t miss, but the patient is not quite aware as to why this can affect that. So, when it comes to malnutrition and cancer treatment, there’s kind of three little buckets, as I think about it. First of all, it’s the patient’s behavior in terms of their food intake and their fluid. Then there’s some subjective measures, maybe there’s how strong the feel, or how much energy they feel. Certainly, strength can be subjective or objective.
So if a patient, if you’re able to measure their strength in the clinic, obviously that’s more objective for most. I mean, in my experience, most dieticians are not measuring strength; it’s really more about the patient can tell, is it harder to go up stairs, is it harder to open doors, is it harder for them to do things that they usually were able to do? And then, their energy level in general. And then the objective measures, if possible, if you can get measure on things like fat stores and muscle stores. And, of course, weight is another objective measure, which would tell us that some of the stores are lost, but we can’t tell just on weight if the weight loss is because of muscle loss or because of fat loss or fluid loss, or whatever it is. So those are a little bit difficult to get to.
What are the causes of malnutrition? So lots of different things, obviously: low appetite; low intake because of side effects; increased nutrition needs, which we’ll talk about how to calculate nutrition needs; if they’re nauseated, if they’re vomiting; if they have a higher metabolism because of the type of cancer or the treatment that they’re getting; if their body’s not absorbing their nutrition. And then their food intake may be low because cancer treatment is very expensive and can be financially toxic to the household budget and therefore they just may not have options in terms of foods, and maybe the foods that they do have access to are not foods that they would tolerate.
So food insecurity is a pretty big issue. At our agency, at Cancer Services, we do a lot of financial assistance, so we have a lot of clients who need assistance with bills and, of course, they’re going to have challenges meeting food needs.
Alright, so when we define malnutrition, there’s a couple of things that we really want to look at, and I think if you think about these things, especially for those of you who have either experience as a cancer patient or a caregiver, or dieticians who work in a cancer center, a lot of the time, you know, this is a pretty big proportion of patients who will meet this malnutrition definition.
So when we talk about moderate malnutrition, that means that they’ve had low calorie consumption for over a month. Cancer generally is considered a chronic condition, so that’s less than 75% of normal intake for a month or more. So usually a patient, you know, may or may not be aware – a caregiver for sure would be aware – as to, well, they’re just not eating as much, well how long as it been. When we talk about acute conditions, that’s really more if somebody maybe has had a surgery or they sort of went downhill really fast. If their intake was low for a week and they have an acute condition, then we would look at them as possible malnourished at that point, and if they have moderate amounts of weight and muscle loss, possibly strength loss.
People are usually, you know, they’re coming into the cancer center, they’re getting weighted on a regular basis, and so likely they are aware as to their weight and whether they’ve lost. So, severe malnutrition is the same only that their calorie intake would be even lower, so less than 50% for five days for either chronic or acute conditions and severe weight loss, essentially. Caregivers, I think, again, are really the best judge at how much somebody might be eating because the patient themselves might not be aware that they’re eating less, because they maybe are eating until they’re full and they’re just full sooner, and so they don’t notice how much food or if they’re eating less food.
And then, from a weight status standpoint, which I think this is a little bit more, this is easier I think for a patient or a caregiver to think about, is just the amount of weight loss. So as dieticians, we look at it and as clinicians, when we’re going to, you know, maybe diagnose somebody with malnutrition, we are going to look at it as a percent weight loss. For caregivers or patients who are on, this is more of a calculation than maybe you’re used to doing in terms of your weight, but you want to do percent weight loss. And what I would suggest is you think about, you may be able to go back to records, but some people, they may not have been weighted until they started coming to the doctor for their cancer treatment or for diagnosis.
I really suggest that people not just what was their weight when they first started treatment, but I would encourage people to think back to what was their weight, sort of their usual weight in adulthood and what was their weight before they started maybe having signs that something was wrong. Because it might be that it took a month or three months from when they started feeling like something wasn’t quite right until they got a diagnosis. And so in that case, we want to go back until what their usual weight was before kind of everything started.
So if I think about a pancreatic cancer patient who, maybe they’ve been losing weight for a month or two before they went to the doctor and figured out that something was really wrong, we want to start with their weight loss the two months prior to when they were diagnosed with pancreatic cancer. So they maybe had lost 20 pounds over those two months. Depending on where they started, we would then calculate the percent weight loss over the time period. So if someone has lost over 5% in a month, or 7.5% in three months, or over 10% in six months or 20 percent over a year’s time, we would consider that severe malnutrition.
Now, it does get a little complicated if somebody in, you know, say a year’s time was also trying to intentionally lose weight, it’s very hard to tease out well what was intentional and what was related to a cancer diagnosis. Just for simplicity’s sake, this is the sort of, the amount that we’re looking at. Now, if you think about your typical patient who’s coming in, a lot of them might meet this guide in terms of malnutrition, so really paying attention to the patient’s experience but also, they may not think it’s as serious as, you know, we as dietitians think it is, so sometimes we have to remind them that this is something they need to be focused on.
And then cachexia is sort of another category of malnutrition, and it’s a little fuzzy because we don’t have clear markers in terms of how to diagnose cachexia, but this is the definition I was able to find. It’s a multifactorial syndrome characterized by an ongoing loss of skeletal muscle mass, with or without loss of fat mass, and so that’s kind of the key that is really a common thread across all of it is this loss of skeletal muscle mass and that it cannot be fully reversed by conventional nutrition support and leads to progressive functional impairment.
So cachexia is something that’s really difficult to treat from a nutritional standpoint; however, up to 80% of patients with advanced cancer may be diagnosed with cancer cachexia, so it is a significant issue. If we can come up with a good strategy of managing and treating it, that’s a different story, but a lot of people are facing this, especially people who have lung, pancreatic, head and neck, or GI cancers and have to go through significant treatments. Those are the ones that are really high at risk for the cachexic syndrome.
Five Tips for Getting Nutrition During Chemo and Cancer Treatment
So, these are my five cancer treatment guidelines to live by: nutrition during treatment strategy. And this is what I kind of give generally, my cancer patient population in terms of, “OK, here are the five things that everybody should really focus on.” And the first one is avoid malnutrition, so we’ll talk a fair amount about that. Eat what you can, when you can; focus on fluids, graze throughout the day; and they get help and support. Those are the five key components to a good nutrition during treatment strategy
So number one, avoid malnutrition, which means get adequate protein and calories. Hands down, the number one goal that we have to avoid malnutrition is to get our patients adequate nutrients, calories, protein during treatment to avoid malnutrition. This is, you know, easier said than done, of course, but that’s one of the key goals. Signs of malnutrition: weight loss, muscle loss, muscle weakness, less energy, easily fatigued, and, you know, not getting enough food in, usually, is the reason behind that.
So this is something that somebody did ask ahead of time, is about screening. A lot of outpatient dieticians have incorporated this really simple screening into their clinics. The challenge is, a lot of people will then, of course, trigger for a nutrition referral, so each center has to figure out, well what score is going to trigger a dietitian referral, depending on how many dieticians you have, and what type of patients you typically see.
I talked to one of the dieticians here in Winston-Salem today and she said that, with a score of two, it was just too many referrals for their dietitians to handle, and so they had to move it up to a three and then try to make sure that they do, like, group education for people like might be at risk but might hit the three level. So, pretty simple if, for those who are patients and caregivers on today, what I would tell you is that these are question – especially caregivers – that you could kind of keep track of throughout the treatment. And really, you know, this is something that I think you could do maybe every week, at least once a month is what I would say from a caregiver standpoint.
This form, what it says basically is, have you recently lost weight without trying? If you’re not sure, that gives you a two, probably because if you’re not sure, then you probably have. So, have you recently lost weight without trying? You get a zero if the answer’s no, and if you’re not sure, you get a two. Now, if you have lost weight, then it calculates points based on how much. So, is it between 2 and 13 pounds? Is it between 14 and 23 pounds? And then it ranks how much those count. So then you have a weight loss score, and then have you been eating poorly because of a decreased appetite, yes or no – yes being one – probably a lot of people are going to score on that, even if it’s not side effects of treatment but it’s just simply anxiety about having cancer that, for a lot of people, is going to decrease their appetite.
So, adding up the appetite score along with the weight loss score is going to give you basically your risk, and then you have to decide. So what I would tell you if you’re, you know, if you’re a dietician, you’re doing these screenings, or you’re having a nurse or radiation therapist who’s doing the screenings, you have to figure out what level you want referred. If you’re a patient, though, what I would tell you is if you are a two or more, I would for sure be talking, I would use the tips – I’ve got some tips on my website – but for sure, if you’re a two or more, number one you need to be in contact with a dietician at your treatment center if they’re available.
If they’re not available and then I would get some information from your medical team – the nurse, probably, or a nurse navigator – in terms of what you might do to either slow down the weight loss or kind of maintain and go the other direction, because we want to recognize if malnutrition is happening early. It’s much more effective to intervene earlier rather than later, because if we start moving towards moderate or severe malnutrition or even moving into cachexia, it’s very difficult to turn that around. So we want to prevent and treat it early on whenever possible. And that’s what these screening tools really help.
So in terms of cachexia treatment, what we do know is that traditional, just like trying to get people to eat more, you know, calories or protein in the foods they eat is unlikely to meet their needs. Because you’ll see in just a minute when I talk about what their calorie and protein needs are, they are significantly higher, and when you think about the typical patient who’s cachectic, it’s also very difficult for those people to eat. So, trying to balance their needs with what they’re actually able to get is going to require oral nutrition supplements at all points of the treatment process and then really troubleshooting which supplement is going to appeal to the patient’s taste to encourage consumption so that they can get in and meet their needs.
So I’ll talk a little bit later about the ENU Nutrition products, which I think is something that will help to add a variety. For some patients, if they’re only consuming oral nutrition supplements or other types of nutrition beverages, they’re going to, you know, need a little bit of variety. So knowing what options are out there so that they’re not just having to drink six, you know, bottles of the same thing every day will help encourage consumption. And then, of course, the entire healthcare team and dietitians could be involved, because sometimes there may be medication management that needs to happen for these people.
This is where I’m kind of moving into how we estimate calorie and protein needs. Now, what I will tell you dietitians, some of you on here are far more experienced in this than I am at this point, because I work mainly in a community setting and in an educational setting, but things have not changed a lot is what I have discovered from when I was working outpatient. What we know for sure is if we’re going to calculate energy needs, of course, for those of us who went through nutrition school, there were all these different ways that you could calculate energy needs, and they’re often not practical.
So, what it comes down to is most, you know, most oncology dietitians are using these simple calculations and then always having to monitor and adjust recommendations based on how it works for the patient. So we start somewhere, and then we monitor how it goes and we change it up as needed. But this is where you can start. So using actual weight, unless their BMI is over 30, and in that case you use ideal body weight. So there was some discussion about using adjusted body weight. I don’t think there’s evidence for using adjusted body weight, so this is where, you know, we’ve landed in terms of what we use.
If they have cancer, they’re inactive, they’re not stressed, then 25 to 30 calories per kilogram is what we calculate. If they are in need of weight gain or repletion, then we would go for 30 to 35 calories, and then if they’re hypermetabolic or cachectic, then we’re going to go up to something like 35 to 40. So those are things to keep in mind when you’re calculating. What I have found is that it’s a lot. I mean, even for somebody to get 25 to 30 who’s just, you know, say they’re kind of doing alright, it still feels like a lot. And our macronutrient breakdown – so in terms of how much of their calories should come from carbohydrate versus fat versus protein is generally the same that we give the overall public.
Which is another reason, I mean, I think all of us who work in oncology have seen some of the articles around cancer and keto, of course, in popular media, the keto diet is still a big thing. I do not think it’s a good idea unless a person has a clear need to adjust their macronutrients to where the fat is really high. I think that if we put somebody, especially somebody who’s at risk for malnutrition or is already malnourished, if we put them on some kind of restrictive diet like keto or even intermittent fasting, I just think it’s going to be really, that’s one more thing that’s going to make it difficult for them to meet their calorie needs, so I’m not a big fan of doing that.
If there’s somebody who’s relatively doing well with treatments, and they can eat, you know, a wide variety of foods and they’re not having appetite issues, that’s a different story, but especially when we’re thinking about malnutrition risk, I do not tend to focus on those types of diets.
Alright, so to calculate protein needs, again, using actual weight or ideal body weight if their BMI is over 30: healthy individuals, 0.8 to 1; generally, for cancer, people going through treatment, that is, 1 to 1.5 (their protein needs are probably a little bit higher); if they’re metabolically stressed but not necessarily cachectic, we go with 1.5; and then if they are cachectic, it would be 1.5 to 2 because they’ve had so much muscle loss and their protein needs are even higher. Again, this is just a place to start, and then you have to monitor. The challenge is, I think, even with calculating these all out, it’s so difficult for people to meet them if they’re not feeling well.
So, I did this just as a sample to kind of remind us how much that actually is. Looking at, you know, in my pretend patient who is five foot eight and 190 pounds, and that’s a BMI of 28, so we’re just going to use their actual weight and, for those of you who aren’t dietitians on the webinar, to change pounds into kilograms, you divide it by 2.2, so 190 divided by 2.2 is 68, and that’s where we get our kilogram body weight. If we’re going to calculate – and I just picked two ranges here – so I picked, let’s compare a general, so let’s say this person is generally doing fine, and so we’re going to do 25 to 30 calories per kilogram versus somebody who’s cachectic and might need 35 to 40 calories per kilogram, so their calorie range would be (for the general person) between 2,100 calories and 2,600 calories.
That’s a fair amount of calories for somebody who’s going through, you now, significant treatment, but let’s say that person’s able to eat pretty well, so hopefully they can meet those needs pretty easily with some of those foods they already like. And then, if somebody is cachectic, we’re talking about 3,000 to 3,500 calories. And I’m just trying to imagine somebody who’s cachectic trying to get that much food in, and that’s why we really need some of these supplements to add extra calories and protein into what they’re already eating so that they can meet those needs.
Alright, so then their protein needs in general, that should say 0.8 to 1.0, and so that’s 68 to 86 grams of protein per day, which, you know, honestly the typical American actually tends to overdo protein already, so for a lot of people, they may already be getting that pretty easily. And then for somebody who’s cachectic, 1.5 to 2, so that’s definitely over what a typical person would be doing. That’s 129 to 172 grams of protein per day. Again, this is a lot for somebody who is typically not feeling well enough to eat, and that’s why we’ve got to figure out strategies to get people to get added calories and protein into their day.
I wanted to do a quick calculation for thinking about, well, how many supplements is that a day. So let me pull up my calculator here. Let’s say somebody needs 3,000 calories a day and they’re getting a supplement drink that’s about 400 calories per bottle, and that’s going on eight to nine bottles a day. I often find with patients that we need to spell it out to them, like exactly what we’re talking about when we’re talking about if we’re giving them calorie recommendations or we’re recommending, “Hey, you need to eat more protein,” like it needs to be specific. If they can’t meet it with their food intake or if they’re eating about half of their calorie needs in food, then they need to keep eating that and add four bottles a day.
Some people I have come in and they’re like, “Well, you know, I had an Ensure or a Boost or, you know, and it tastes OK, but I don’t like it that much, so I just have one a day.” That’s something, but probably they’re going to need more, so helping them to figure out what kind of volume are we talking about will meet these needs. That, I think, can help. It helps a caregiver kind of get some framework around estimating what they’re getting, but it also helps the patient realize how much they’re probably going to need in order to either prevent malnutrition or feel a little bit better.
Number two on my five tips is to eat what you can, when you can. Someone’s asking, “What’s your reference for using ideal body weight?” I think that that is in the oncology nutrition book, and I can’t remember the name, the actual name, but it was out in 2013. They are working on a new updated version that hopefully will be out beginning of 2021. So that is where we’ve been able to find that. And if you are a member of the oncology nutrition practice group, that’s a great place to ask too. OK, so good question.
So, back to number two, eat what you can, when you can. Reminding patients to eat foods that sound good and appetizing, eat something every two to three hours. You can eat more healthy things on the days that they feel well and choose to meal prep specific foods that can help with symptoms or ask friends and family to do that. Find strategies to meet needs despite eating challenges, and we’ll talk briefly about some of the eating challenges, but really, strategizing around that.
Focus on fluids; dehydration is a huge problem, especially when it comes to maintaining nutrition status, not missing treatments, and also feeling well and energized is to stay hydrated. So if water is not a great option, herbal tea, juice, lemonade, sparkling water, broth, sports drinks, Pedialyte, all those types of things. The dietitian I talked to today, she said they use Pedialyte popsicles. You can do all kinds of things, but just kind of trying to get those fluids in. If people aren’t able to get their fluids in, obviously they can get IV fluids if needed. But, you know, medication management is something that’s really huge, so if somebody’s having a lot of diarrhea or vomiting – which is going to contribute to dehydration – we probably need to get some meds on board that will help them keep it down.
Grazing: So, my general rules – and these are not in anybody’s books – these are just my common sense tips, is to eat within one hour of waking and eat something every two to three hours throughout the day. And this is true for liquids and foods. This is just my general common sense rule for people, don’t waste any time during the day. That getting up in the morning, taking meds on an empty stomach, and then eating an hour after that, I think, is the best option. And then something every two to three hours, and that way, if they’re up for 12 hours, they’re going to get several mini-meals in, and if we can calculate like a target goal of calories per little meal, that will help them to really think through what might work for them.
Obviously, higher calorie, higher protein meals or snacks mean that they don’t have to eat as much food at a time, which is often helpful. Maximize meals and snacks by including calorie- and protein-dense foods.
Alright, and number five is “Get help and support.” I think a lot of times, we as dietitians don’t always help our patients optimize, sort of the support team that they may have available around them. Of course, by the time they reach us, as dietitians, they’ve probably been through a lot of people, because sometimes we’re hard to find. But ideally, the patient will know who their medical team is, who’s on their, you know, who can they call when they need something. I often have to just encourage people, they like, they don’t want to bother their medical team. And I’m like, “You’re paying for it,” you know. Nobody’s bothering anybody; that’s what they’re there for. So really encouraging them to speak up if they notice that they’re losing weight and somebody hasn’t brought that out to them.
Have a social support system identified. Figure out who in your social circle, either living in your household, neighbors, you know, church friends, or whoever is in your social circle and is willing to help and identify jobs for each of them. Some of those people might be really great at cooking, and some of them might just be good for mowing the lawn, but really figuring that out so that you can identify someone who’s going to support you during treatment days, which may also be the same person who helps you get adequate nutrition, especially on that day.
But also, I think having somebody who is kind of a good encourager, not a food pusher or somebody who’s going to guilt you about any of the food that you are choosing, but rather somebody who’s on board with your nutrition strategy who can help remind you when it’s time to eat. Those are the people that you want to kind of be keyed into what it is that your nutrition needs are.
And then, financial assistance for food insecurity or other bills so that you can make sure that you have access to the foods that you need. So somebody’s asking, “Morning meds on an empty stomach or after eating?” It depends on the medication, but sometimes what I hear from people who skip meals, like say they skip breakfast, is that they say, “Well, I have to take my medicine on an empty stomach,” so if they have medication that they have to take on an empty stomach, then it counts as either doing that an hour before eating or two hours after eating.
Now, if you’re thinking about eating every two to three hours during the day, it becomes like this logistical nightmare to try to figure out when can you take your empty stomach medication, because you have to eat and then wait two hours and then take the medication, and then you can’t eat again for another hour. So I find the simplest thing for those people, if it lines up with their medication schedule, to take their “empty stomach medicine,” if at all possible, first thing in the morning or possibly last thing at night before they go to bed. But obviously, if they have medication that they have to take with food, they can kind of do that whenever it works.
For people who are on nausea medicine, I always remind them that we want to take that 30 minutes before they plan to eat so that it’s kicked in and working rather than waiting until they sit down to eat and then things are kind of, they don’t feel well. It takes 30 minutes for it to kick in, and then they don’t really feel like eating and all their food is, you know, old, and their family’s already done, so really planning ahead for that.
OK, and some other people made some comments about estimating needs, and I would say, for anybody who is a dietitian, of course you can use all kinds of different calculations; however, I’ve found, you know, you can calculate with all kinds of calculations. Yes. For patients who are interested in calculating needs, probably not going to use equations as much as even if we can get them to kind of just think about the calories.
Cancer Treatment Side Effects
Alright, so what are some common cancer treatment side effects? I’m not going to spend a lot of time on this, but this is often how I explain it to my clients. First of all, we need to deal with the symptoms that are causing their reduced calorie intake. So, do they have a poor appetite? Is it, you know, fatigue, constipation, diarrhea, nausea, taste and smell changes, sore throat, and mouth? Like, what is it that’s preventing them from being able to eat enough to meet their calorie needs? And so, once we can identify those symptoms that are causing problems, can we address them with medication, and can we come up with a nutrition strategy that makes it possible for them to eat foods?
And it’s hard, you know, it’s just really hard for people to figure out, to make themselves eat multiple times a day when it doesn’t feel good. But if at all we can figure out how to get those nutrition needs met, that’s what we’re going for. So for caregivers and patients who are really in the middle of this, that’s what we’re encouraging, is to figure out, you know, what’s contributing to this problem and then look at various ways to improve that, because if we can manage the symptoms and get enough calories and protein, and your nutrition status is better, you have improved outcomes. You’re happier. Your medical team’s happier.
And I do have some, I’m not going to spend a lot of time right now, or any more time, specifically on any certain treatments or side effects. First of all, I did a webinar earlier in November, specifically around treatment side effects and some of these strategies we use to manage those, so you can always go onto this website, which is cancerdietitian.com/tips. On that page, I have links to different side effects and what you can do to help with those. And also at the bottom of that same page is the, you can watch the video recording of my webinar I did earlier this month, which really focuses more on these side effects.
And then if you are wanting a printable kind of version, we give these out at our office at Cancer Services, so if you’re in our local area, I can get these for you, but if you’re somebody who would like to have a printed resource with some of these tips, you can download through the store on my website. And I did make a coupon code for anyone who’s attending today, if you want to download that booklet. If you’re a dietitian and you want to download it, it’s fine for you to use it within your treatment center, but please don’t send it outside of your treatment center. So that’s just an option if you want a printable resource.
Nutrition Drinks and Supplements for Cancer Care and Chemotherapy from ENU
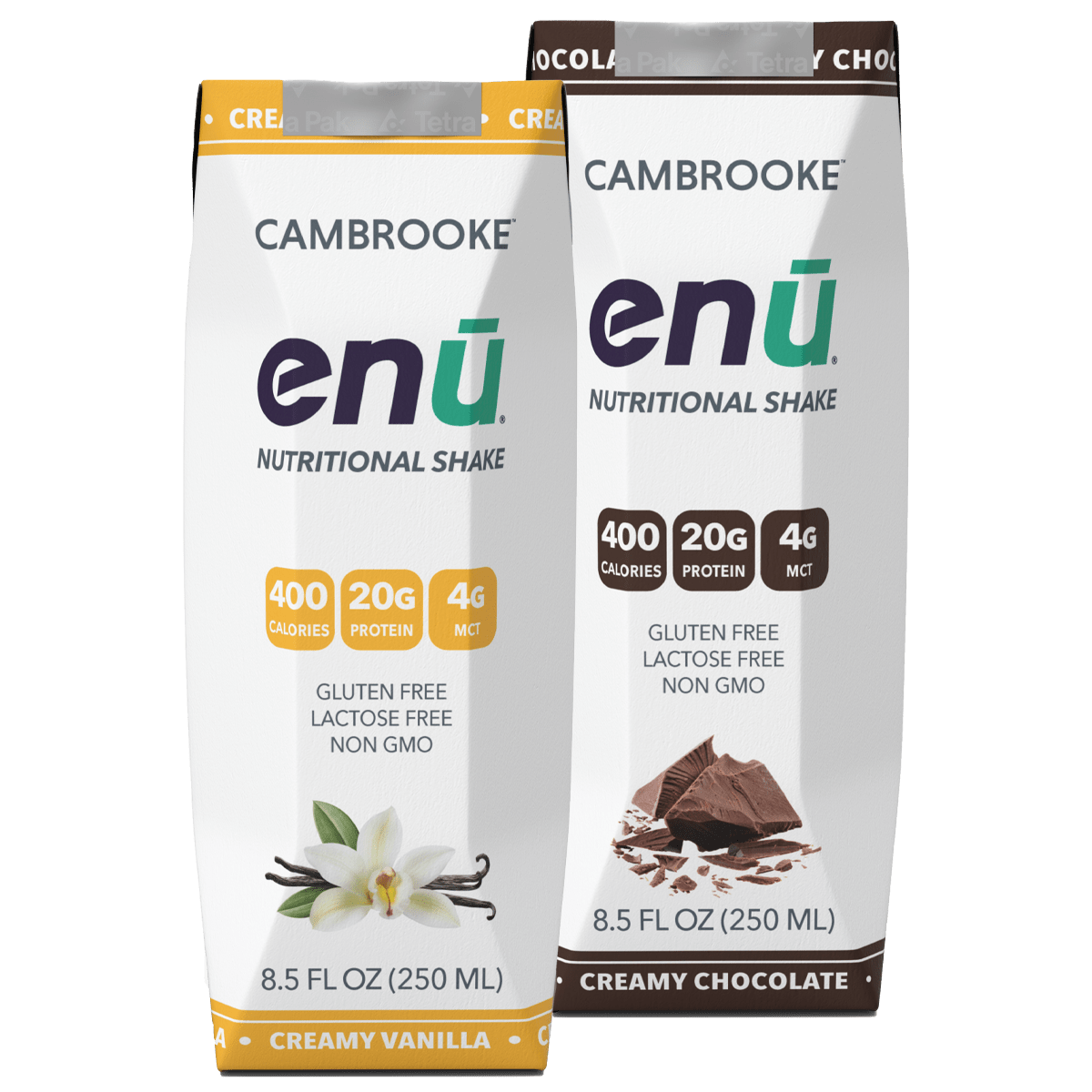
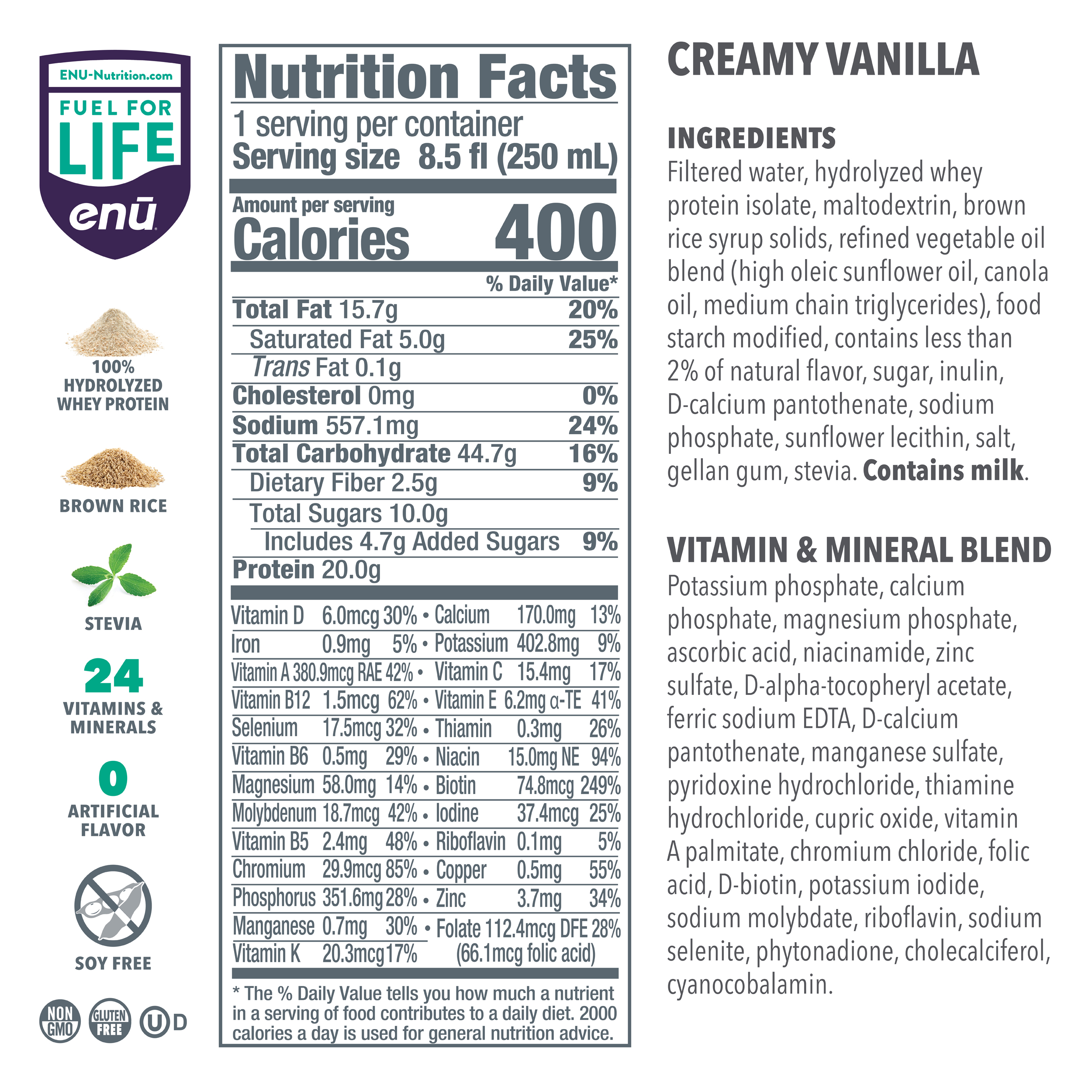
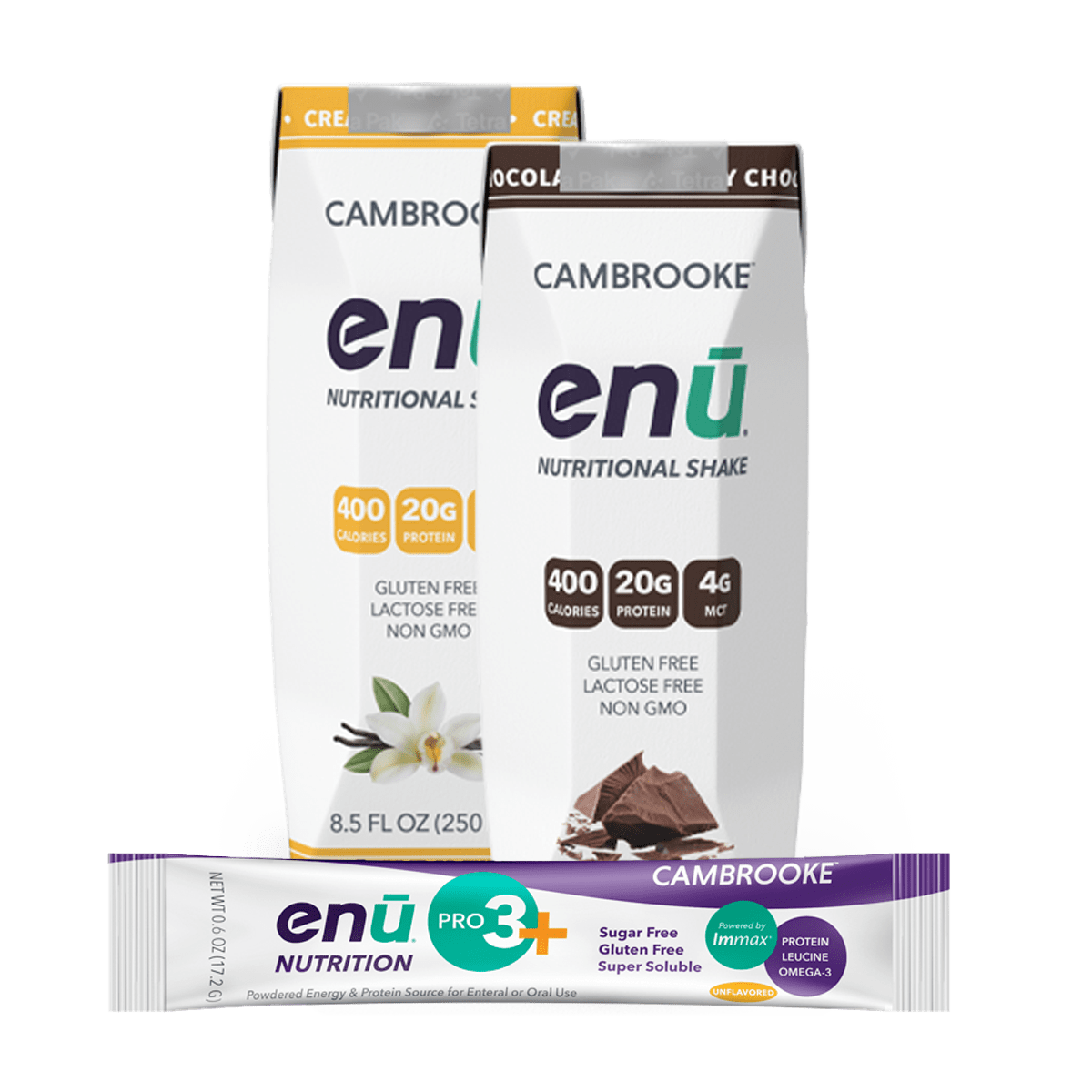
OK, so what I do want to highlight is our sponsor for today, ENU Nutrition has two different products that I think can be helpful, especially when we think about cancer cachexia and the idea that of course everybody needs to be using a nutrition supplement of some sort, and that they may not tolerate or enjoy some of the flavors of some of the ones that they’ve already tried, that this can be a product that may be something different for them.
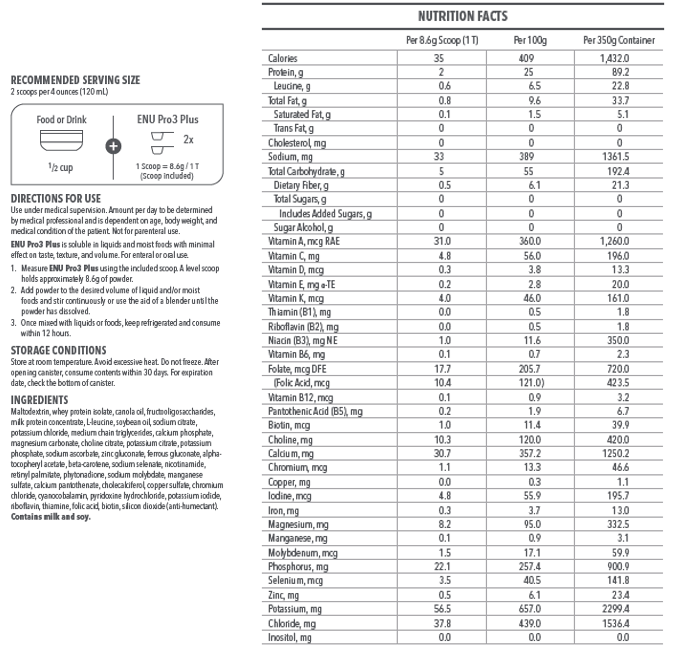
So, two things that ENU Nutrition offers: one is this powder. It has calories and protein built into it, and in the protein, they’ve focused on leucine because of how it supported muscle growth and also omega-3s, which there is some data showing that omega-3 can help combat some of the inflammatory and cachectic-type metabolic issues that are going on in the body.
So someone had asked ahead of time about that. I don’t have a lot of data on that; I think it’s something that we think can be helpful, and certainly other products are starting to add omega-3s into their products. So I think it’s worth, you know, it’s certainly not going to hurt. And so having products that have omega-3s in them may be especially beneficial for some of the more hyper-metabolic situations.
So two things: that’s the shakes that they have in containers there, you can see, and then this powder which is a flavorless powder that you can add to all different kinds of things. They are specifically designed for cancer patients and those who are at risk for malnutrition and cachexia and also can be beneficial for the elderly, especially because the elderly tend to have more muscle breakdown. So they are helpful for both of those situations, and they help to increase protein and nutrient intake, especially the powder that’s really easy to add to a lot of different things.
Any dietitians or clinicians, you can get bulk samples. Their website is enu-nutrition.com, pretty simple. If you want, I can connect you to some of their people to get samples. But patients can also get samples from their websites, you just have to pay, I think it’s like two dollars shipping and they’ll send you some samples of the powder as well as the drink. You can purchase them on their website; they’re also available on Amazon and Walmart for online shopping.
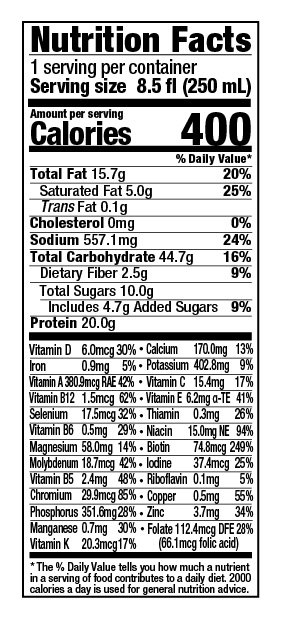
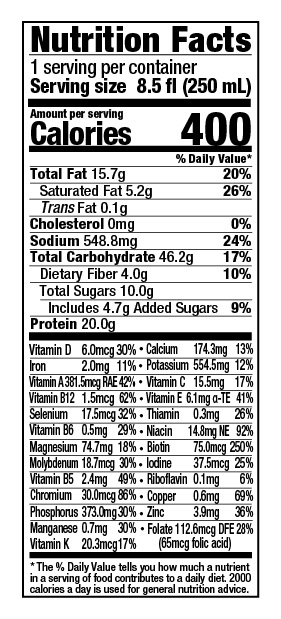
I mentioned it has protein, omega-3s, and leucine, along with calories in this particular product. Good palatability, which is really beneficial, especially, I mean I know patients who the sweet flavor of some of the supplement drinks just doesn’t work for them. And so this is a way that you can add calories and protein into foods that are necessarily sweet. So it can really enhance the nutrition value of some of the foods that they already eat. No participants in their trials found negative side effects. They don’t interfere with most cancer treatments. It’s formulated to meet specific needs of cancer patients. The protein powder, or it’s also calories, can be added to tube feeding as well. So if they are on a tube feeding that they tolerate and they just need a little bit more added to it, this is an option as well.
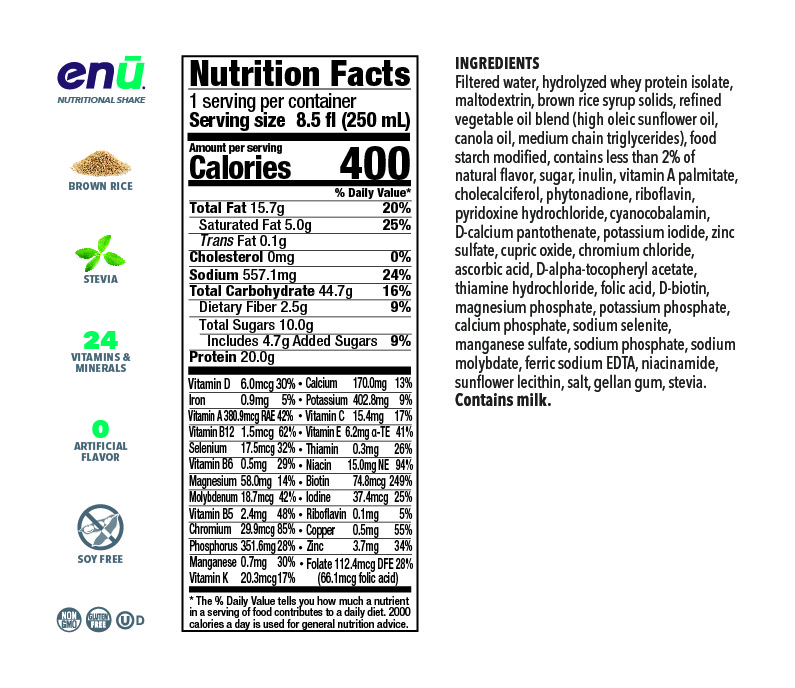
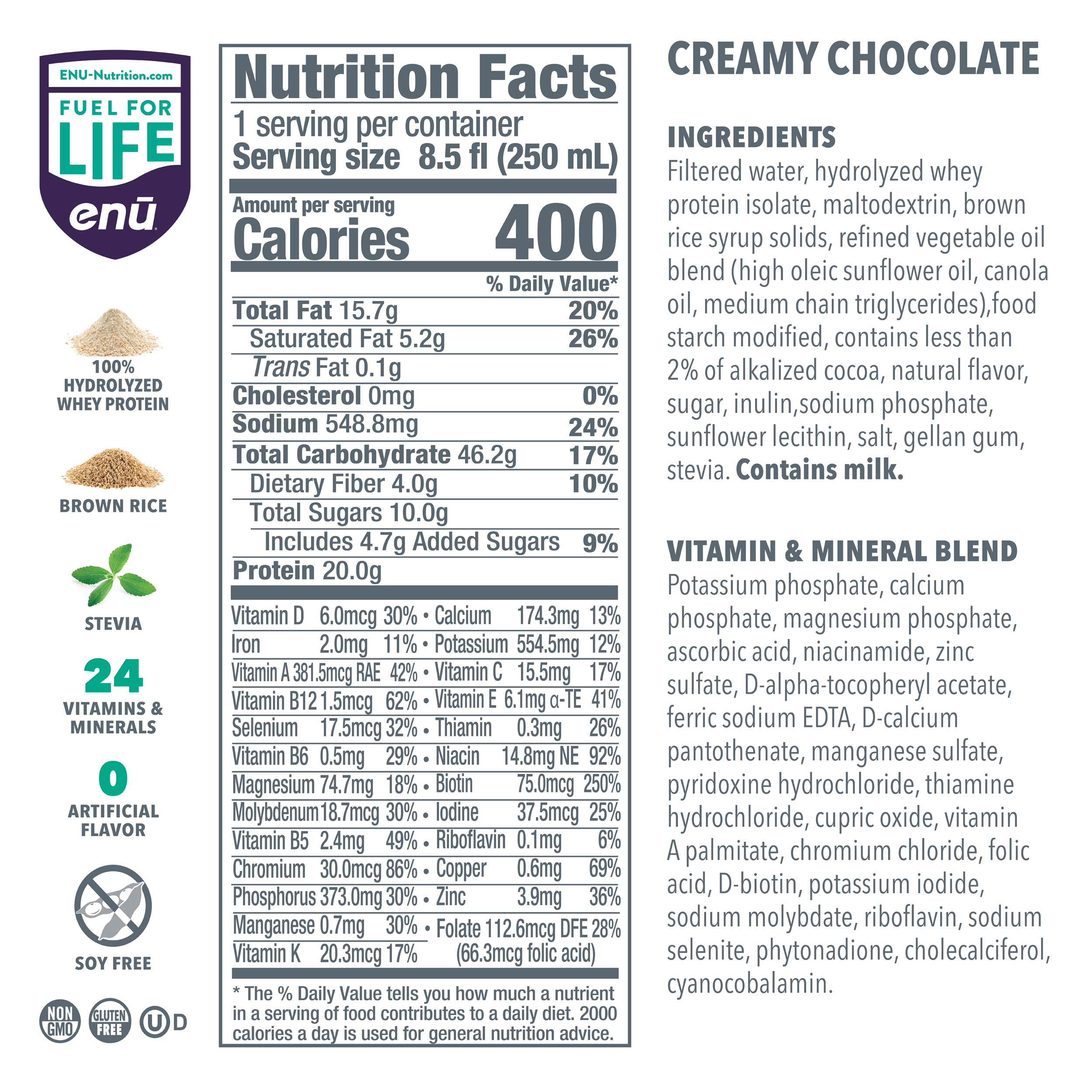
Let’s see. So here is some of the information. The sweeteners that they add to enhance the carbohydrate content tend to be more complex carbohydrates than sugar, so a lot of people like that. It does have some fiber, also beneficial. It has 400 calories per serving and 20 grams of protein per drink, which is pretty calorie- and protein-dense, which is handy. And also, when you think about how much calories you’re getting per dollar or protein per dollar, I always tell people to go for the most that they can get. But also, you can thin it down yourself at home and that can help save you some money.
And then the powder easily mixes into all kinds of food and beverages without changing taste or texture. So I don’t think they have anything specific that they would recommend that you use it with, just whatever you’re going to tolerate, maybe that you already know.
So they worked with oncology doctors and dietitians to develop the product. Very helpful, they’ve tested it among patients, so you can see that. Better taste and mouth feel. A lot of them felt like they focused on the leucine, the omega-3s in there. And then when they compared their group to control, they found an increase in daily protein and calorie consumption almost, you know, over 25%. So that’s really good.
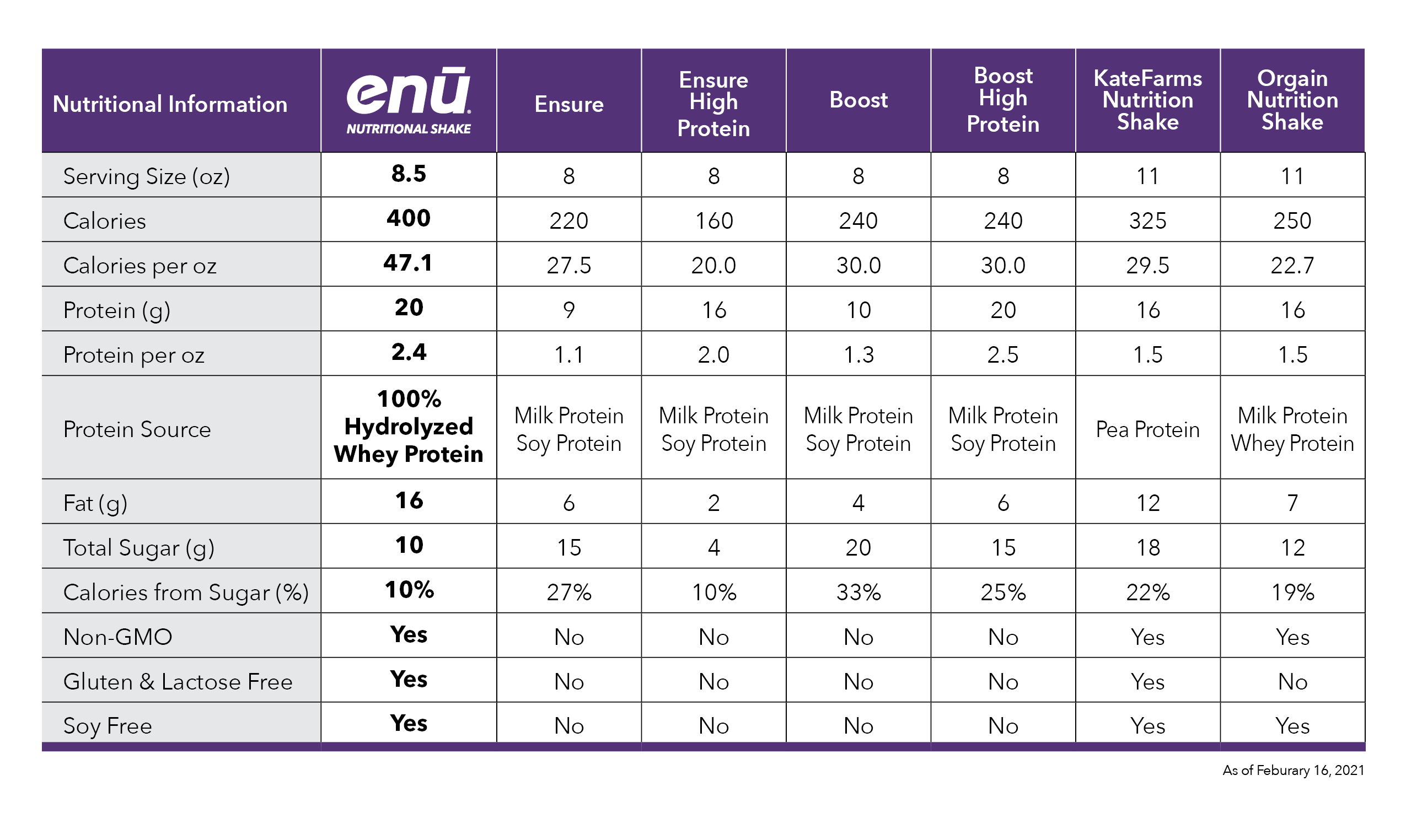
I think this is a great option, especially for people who’ve tried other things and really haven’t liked the flavors, to be able to mix this in. I know there are some other mix-in type of products, which I’ll talk about in a minute, but this is just how it compares. And this is comparing it to the basic Ensure product, the basic Boost product, and then Kate Farms and Orgain are other ones that I’ve had patients, also, they’re used to getting. They can either get that at the store or they order it online.
So, per fluid ounce of just the regular versions of these things, ENU, the product has more protein pre fluid ounce. The cost per gram of protein is also my more affordable in this case. Calories per fluid ounce is higher. And then the percent calories from sugar, which is, you know, what people can sometimes complain about the overly sweet flavor of some of them, because they’re using more of a complex carbohydrate in their product, it’s not going to have the same overly sweet taste. So I think that’s a benefit for people who comment that that’s not meeting their flavor palette.
So to compare the powders to Duocal or Benecalorie, you can kind of see the nice thing about the ENU powder. It’s a little fewer calories than the Benecalorie, but it does have a significant amount of protein added to it. So that’s something to really keep in mind. And you can mix it with anything, and then the protein source is whey protein isolate, milk protein concentrate, and then they have that leucine in there. It does contain fiber, which is another helpful – I think it’s helpful – to have in the product.
And then, I thought this was interesting as well. So if you’re thinking about how much leucine you can get in different foods, let’s say that you’re trying to get a patient to meet their protein needs, and they’re going to use this product for part of their needs but not all of their needs. Here’s some other comparisons in terms of the leucine content of other foods. Us dietitians, we love food comparison charts. So just thinking about, if we’re talking about muscle protein synthesis, looking at 25 to 30 grams of protein per meal – which is generally what we recommend – that this would be the amount of leucine that someone could get in a typical meal. And that what you get in six scoops of the powder is actually similar to what you might get in some kind of real food option. Although, that’s a lot of eggs on here. Six eggs to give you 3,000 mg of leucine.
What is the cost? That’s the other big issue, especially for people who are in treatment. They’re paying their medical bills and they’re like, you know, I can’t afford things. So a couple of options for this. For sure, if you’re a clinician, you should just get some samples so that people can try them before they purchase them. Or, if you’re a patient, you can order the free sample pack. That’s helpful. I’ve had that sent to a couple of our clients here at cancer services.
If you do end up purchasing, you can get 20% off of your first order if you use either my specific affiliate link, which is enu-nutrition.com/julie – that’ll automatically apply the coupon – or you can go in and enter “JULIE” as the coupon code. But you want to check around, so check the ENU Nutrition site and, yes, if you buy there, then 5% does come to support the programs at Cancer Services, so it doesn’t, you know, fluff my pocket, but it does help us as a nonprofit to be able to continue offering services. But, check Amazon, because I think that Amazon had a pretty good deal on these that might be cheaper than actually going through the website.
So always, I’m a frugal shopper, so I say check different websites. Amazon, Walmart.com, and enu-nutrition.com/julie and see which, you know, the best deal, if you do want to purchase them. Let’s say you tried the sample pack and you feel like it’s helpful. And then you can also buy in bulk the powder and also the shake. So, as I understand it, this is actually a better price than what you can get for sure than what you can get for, like, some of the other products that you buy just at the store in a six-pack, because those are really expensive.
So this can be more cost-effective than some of the commercialized products that are more available, so that’s something that you want to know about. And if you buy them by the, you know, case, that’s also helpful. And always check for coupons, coupon codes wherever you go.
Common Questions About Nutrition During Cancer Treatment
Alright, so that is kind of the end of the general information. I do want to address some of the questions that came in ahead of time, and then some of the ones that have, I think I’ve answered all the ones that have come through so far today. So if you’re not familiar with the website, I have the cancerdietitian.com website as well as Cancer Dietitian podcase episodes What I want to do now is to address the questions that came in ahead of time, and then if you have other questions, go ahead and put them in the Q&A box.
So, somebody asking about the fish oil to help with muscle mass and weight. I don’t have a lot of success on that. I think that they theory is pretty good, and that’s why products are adding omega-3s. It can be hard for people to tolerate sometimes, but what I have found is that using some of the liquids rather than the pills can get them more of the omega-3s per volume. Some of the Nordic Naturals that have the lemon flavor is easier to tolerate.
Any tips or tricks for people with low BMI but eating well? I think that generally, just getting them their nutrition recommendations and helping them understand how much food that really is. I think people with low BMI are often pretty aware that they don’t have many stores and so just reminding them that we want to keep those stores built up. But it is hard. If they’re not motivated to increase their nutrition intake, what I say is, you know, we do our jobs as dietitians – and caregivers have the same challenge – is, you know, if you want your loved one to eat more, but your loved one does not want to eat more, you can’t force the food down their throat. And adding a lot of anxiety around mealtimes is not going to help the issue.
So what I would often tell caregivers, and what I would say this to dietitians too, is you have a role, and then there’s this boundary where your role stops and the patient’s role begins, and it’s up to the patient whether they take your advice or you’re, you know, gentle nudging as a caregiver or not. And it’s really hard but, you know, we can’t make them do it. So I don’t suggest that you as a caregiver or a dietitian or a food pusher or guilting people about things.
Giving them the tools and asking them what else they need to help them along the process, but then whatever choice they make, you know, if they choose, they don’t feel like eating it and they can’t make themselves eat it, I tend to have a little bit more, you know, grace and compassion for those people and hope that maybe they’ll be able to pick up a few more calories here and there on a different day.
And then, for the patients who have sort of had maybe a dieting mentality over their life and then they get diagnosed with cancer and now they have weight loss and they’re kind of maybe happy about it. That’s a hard one as well. What I would say is if they’re educated as to what the risks are of malnutrition and you’ve given them the tools to meet their nutrition needs. Now when you calculate their needs, that might be something you just kind of keep in mind.
So in the discussion around how do you calculate their needs, if this is somebody whose BMI is above 30, and you’re calculating it based on ideal body weight or you’re using one of the fancy calculations, it’s probably going to be a little bit harder for them to even consider some of the higher calorie levels. So what you might do in that case is, rather than telling them how many calories to eat is to actually try to estimate how many calories they’re currently eating and then just encourage them to add maybe 150 or 200 or 300 more calories in a day, and then monitor their weight and see if that helps.
They can also monitor their symptoms and they may find what might help is if they’re monitoring what they feel like, their fatigue, or their energy level, and you know kind of things like that, the things that they want, they want to sleep well, they want to have energy, they want to have good treatment outcomes. If they can monitor their energy level and if we can somehow tie that they feel better when they eat better, then that’s going to be more motivating than saying that, “Well, your weight’s down and we want it up,” because if they don’t value having their weight at a certain level, then they’re not going to play the game.
But if they value having good energy, then that’s the angle that I would come at is, you know, when we meet your needs – and helping them remember that a calorie is just a measure of energy – so if rather than calling things calories, and we talk about it as energy, like, “I need to you eat enough energy, I need you to eat enough food to fuel the energy that you want to live a good life during treatment,” that sometimes can communicate just a little bit differently and they might be more motivated.
And then, this is also an interesting comment that someone sent. People who always enjoyed food (maybe sometimes too much) – like they, foodies, they love food, they just enjoy every bite – are least able to power through because the food isn’t enjoyable. And so those who have been more “eat to live” do a better job of maintaining status, which I think that all comes down to our relationship with food.
And we all have kind of complicated relationships with food, but for sure, there’s people who, they just eat to live, and then there’s other people who live to eat. And usually they can identify that, so it is hard for people who have this emotional tie to their food when it doesn’t taste right, that it’s painful.
That’s like, you get your feelings hurt because what used to make you really kind of feel good, or say you’re the cook in the family and you just don’t feel like cooking anymore and that was how you loved your family, to find other ways to meet that need and then to also help them see that this really is kind of like a medication, that their nutrition intake is like medicine. That it will help them to feel better, and it will help them to tolerate the treatment and to get back to the way they wanted their relationship with food to be, assuming you think that it’s going to get to that place.
I also very much rely on the other team members in the care team, and that would be the counselors, the social workers. It might be that really working as a pair with the counselors or the social workers to help people meet those needs can be helpful. It might be that, if it’s a behavior issue and they’re a counselor at the cancer center, that you can give the counselor some of the nutrition tips and say, “Can you see this patient, because I need them, their behaviors to be worked on rather than just their nutrition.” So that’s my take on that.
What other questions do you all have? Suggestions on using the powder in cooking. I think you can use it in cooking. I have not tried it that way, but that is something if, I have your email, so I may actually ask that question of the ENU people and see if they have recipes or things that can be useful for that. Let me make a note. I think mostly it’s been used as a mix-in, but that’s a good question.
Somebody did ask about resources for studying for the oncology certification exam, and if you are not aware, the oncology nutrition practice group is actually offering a session, a three-part session in January that you should definitely sign up for. It’s essentially kind of like a prep course. So that’s on oncologynutrition.org. You can find information about that. “Fundamentals” or something is the course.
What would the nutritional percentages of a hamburger be in relation to protein, carbon, fat? So when we’re looking at the recommendations for percent of calories to come from carbohydrate, it’s a little bit complicated because it’s not of the individual food that we want that percentage to be; it’s kind of your overall dietary pattern. So you might look at it from a day or a week’s perspective, so it’s not any one particular food that needs to meet those guidelines. It’s just the combination.
So what I would tell you, from a patient’s standpoint, it’s not really useful to calculate those things. What I tell my patients is that, by eating just a good variety of foods, you’re going to meet those needs. If, however, you’re on like a tube-feeding or you’re getting your nutrition from nutrition supplements a lot of the time, that’s when you’re going to definitely want a dietitian to calculate that up for you and make sure that you’re meeting those needs.
Anything else? Oh good, somebody put in the chat that there’s recipes on the ENU Nutrition website, so make sure that you use those. I’m going to put that in the chat. And if you go over there, if you try them or you have patients try them, let me know what you think their favorite is.
So yeah, I think that’s it, unless people have any other questions. I will put this recording up on the Cancer Dietitian website, so you can make sure that you sign up for the updates that’ll go out by email to let you know it’s ready. I’ll share a copy of the slides on there for download, have links on there, and then also make sure that you have access to the recording. If you have any other questions, feel free to email me, contact me, let me know what you think, and I would be happy to send over whatever you need. Thanks so much everyone! Have a great day. Stay healthy and well.
Protein Shakes for Cancer Patients from ENU Can Help You Get the Nutrition You Need
If you or a loved one is going through chemotherapy or other cancer treatment, place an order with ENU today for nutritional supplements like our meal replacement shakes or Pro3+ nutritional powder to ensure they get the nutrition they need during their care.